Japan and South Korea Data Raise New Concerns Over mRNA Safety
A new study and raw data from East Asia are raising fresh concerns about the “safe and effective” mRNA injections.
A large South Korean cohort study found links between COVID-19 vaccination and higher rates of several cancers at one year follow-ups. And, an independent Japanese data effort—now public online—shows an unusual rise in all-cause deaths roughly three to four months after many mRNA shots. Together, these reports do not prove a causal link, but they do show patterns public health agencies should not ignore.
A South Korea study, published in Biomarker Research, looked at health records for millions of people to see whether cancer incidence changed in the year after COVID-19 vaccination. After matching vaccinated and unvaccinated groups, the authors reported higher hazards for six cancers—thyroid, gastric, colorectal, lung, breast and prostate—with hazard ratios ranging from about 1.2 to 1.7 depending on the cancer type. The paper is careful to call these findings “associations,” and the authors call for more work to explore possible causes. Still, the large size of the dataset and the consistency across cancer types make the result hard to ignore.
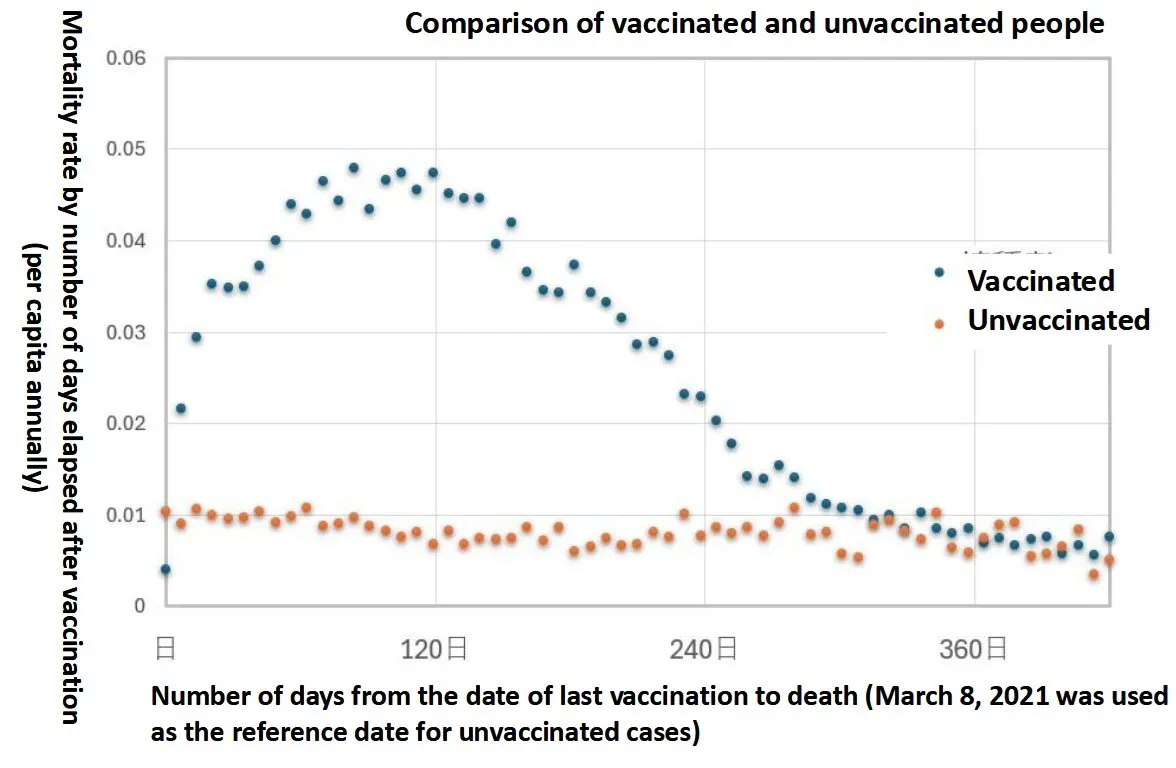
In Japan, a citizen-led project obtained millions of local vaccination records via public-records requests. Researchers there aggregated batch numbers, dates, age groups and whether the person later died. Their analysis found a striking pattern: rather than a spike in deaths immediately after injection, the largest rise in all-cause mortality showed up around 90–120 days later—roughly three to four months after many doses. The team reports that more doses were linked to earlier and sharper mortality peaks, and that some lots showed much higher rates than others. The dataset and the team’s write-ups are public.
The implications of the Japanese data are clear: if a real risk shows up two to four months after a shot, short-term safety checks that look only at events in the first few weeks will miss it. The Japanese group argues that current surveillance systems are blind to that kind of delayed harm. They call for a full review and for regulators to release the raw records so other independent teams can test and try to reproduce the finding.
As always, careful reading matters. The South Korea authors note limits to their study: observational data, possible residual bias, and that a statistical link is not the same as proof. The Japanese effort is raw-data driven and striking, but it is not (yet) the same as a peer-reviewed causal study. Still, both lines of evidence point in the same direction—delayed signals that warrant urgent, transparent study. Regulators should not be allowed to treat such signals as minor or anecdotal.
These studies add to the growing body of evidence that the mRNA injections—which required an “update” to the definition of “vaccine” to be labeled as such—are, in fact, neither safe nor effective. They add weight to recent decisions by the FDA to rescind emergency use authorization and the CDC to drastically alter recommendations for mRNA injection use from “everyone” to those most at risk, based on personal choice.
Both studies also highlight the necessity for ongoing, long-term follow-up of those who received these injections, to further investigate their effects on overall mortality and cancer rates, but also their association with decreased fertility, increasing infant mortality, increased stillbirths, and numerous other serious conditions and adverse outcomes.
Given their lack of protective efficacy and significant risks, it can be argued that the CDC’s decision was perhaps too conservative in that they allowed the continued use of mRNA injections, rather than the immediate market withdrawal some have demanded. However, the South Korean and Japanese reports add additional cautions to the “personal choice” discussions that are now the standard of care in America.